Urine contains many dissolved minerals and salts. When your urine has high levels of these minerals and salts, you can form stones. Kidney stones can start small but can grow larger in size, even filling the inner hollow structures of the kidney. Some stones stay in the kidney, and do not cause any problems. Sometimes, the kidney stone can travel down the ureter, the tube between the kidney and the bladder. If the stone reaches the bladder, it can be passed out of the body in urine. If the stone becomes lodged in the ureter, it blocks the urine flow from that kidney and causes pain.
The Kidneys and Urinary System
The kidneys are fist-size organs that handle the body’s fluid and chemical levels. Most people have two kidneys, one on each side of the spine behind the liver, stomach, pancreas and intestines. Healthy kidneys clean waste from the blood and remove it in the urine. They control the levels of sodium, potassium and calcium in the blood.
The kidneys, ureters and bladder are part of your urinary tract. The urinary tract makes, transports, and stores urine in the body. The kidneys make urine from water and your body’s waste. The urine then travels down the ureters into the bladder, where it is stored. Urine leaves your body through the urethra.
Kidney stones form in the kidney. Some stones move from the kidney into the ureter. The ureters are tubes leading from the kidneys to the bladder. If a stone leaves the kidney and gets stuck in the ureter, it is called a ureteral stone.

What are Kidney Stones Made of?
Kidney stones come in many different types and colors. How you treat them and stop new stones from forming depends on what type of stone you have.
Calcium stones (80 percent of stones)
Calcium stones are the most common type of kidney stone. There are two types of calcium stones: calcium oxalate and calcium phosphate. Calcium oxalate is by far the most common type of calcium stone. Some people have too much calcium in their urine, raising their risk of calcium stones. Even with normal amounts of calcium in the urine, calcium stones may form for other reasons.
Uric acid stones (5-10 percent of stones)
Uric acid is a waste product that comes from chemical changes in the body. Uric acid crystals do not dissolve well in acidic urine and instead will form a uric acid stone. Having acidic urine may come from:
- Being overweight
- Chronic diarrhea
- Type 2 diabetes (high blood sugar)
- Gout
- A diet that is high in animal protein and low in fruits and vegetables
Struvite/infection stones (10 percent of stones)
Struvite stones are not a common type of stone. These stones are related to chronic urinary tract infections (UTIs). Some bacteria make the urine less acidic and more basic or alkaline. Magnesium ammonium phosphate (struvite) stones form in alkaline urine. These stones are often large, with branches, and they often grow very fast.
People who get chronic UTIs, such as those with long-term tubes in their kidneys or bladders, or people with poor bladder emptying due to neurologic disorders (paralysis, multiple sclerosis, and spina bifida) are at the highest risk for developing these stones.
Cystine stones (less than 1 percent of stones)
Cystine is an amino acid that is in certain foods; it is one of the building blocks of protein. Cystinuria (too much cystine in the urine) is a rare, inherited metabolic disorder. It is when the kidneys do not reabsorb cystine from the urine. When high amounts of cystine are in the urine, it causes stones to form. Cystine stones often start to form in childhood.
Symptoms
Common symptoms of kidney stones include a sharp, cramping pain in the back and side. This feeling often moves to the lower abdomen or groin. The pain often starts suddenly and comes in waves. It can come and go as the body tries to get rid of the stone.
other signs of a kidney stone include:
- A feeling of intense need to urinate.
- Urinating more often or a burning feeling during urination.
- Urine that is dark or red due to blood. Sometimes urine has only small amounts of red blood cells that can’t be seen with the naked eye.
- Nausea and vomiting.
- For men, you may feel pain at the tip of the penis.
Causes
Low Urine Volume
A major risk factor for kidney stones is constant low urine volume. Low urine volume may come from dehydration (loss of body fluids) from hard exercise, working or living in a hot place, or not drinking enough fluids. When urine volume is low, urine is concentrated and dark in color. Concentrated urine means there is less fluid to keep salts dissolved. Increasing fluid intake will dilute the salts in your urine. By doing this, you may reduce your risk of stones forming.
Adults who form stones should drink enough fluid to make at least 2.5 liters (⅔ gallon) of urine every day. On average, this will take about 3 liters (100 ounces) of fluid intake per day. While water is likely the best fluid to drink, what matters most is getting enough fluid.
Diet
Diet can also affect the chance of forming a stone. One of the more common causes of calcium kidney stones is high levels of calcium in the urine. High urine calcium levels may be due to the way your body handles calcium. It is not always due to how much calcium you eat. Lowering the amount of calcium in your diet rarely stops stones from forming. Studies have shown that restricting dietary calcium can be bad for bone health and may increase kidney stone risk. Health care providers usually do not tell people to limit dietary calcium in order to lower urine calcium. But calcium intake should not be too high.
Instead of lowering dietary calcium intake, your health care provider may try to reduce your urine calcium level by decreasing your sodium (salt) intake. Too much salt in the diet is a risk factor for calcium stones. This is because too much salt is passing into the urine, keeping calcium from being reabsorbed from the urine and into the blood. Reducing salt in the diet lowers urine calcium, making it less likely for calcium stones to form.
Because oxalate is a component of the most common type of kidney stone (calcium oxalate), eating foods rich in oxalate can raise your risk of forming these stones.
A diet high in animal protein, such as beef, fish, chicken and pork, can raise the acid levels in the body and in the urine. High acid levels make it easier for calcium oxalate and uric acid stones to form. The breakdown of meat into uric acid also raises the chance that both calcium and uric acid stones will form.
Bowel Conditions
Certain bowel conditions that cause diarrhea (such as Crohn’s Disease or ulcerative colitis) or surgeries (such as gastric bypass surgery) can raise the risk of forming calcium oxalate kidney stones. Diarrhea may result in loss of large amounts of fluid from the body, lowering urine volume. Your body may also absorb excessive oxalate from the intestine, resulting in more oxalate in your urine. Both low urine volume and high levels of urine oxalate can help to cause calcium oxalate kidney stone formation.
Obesity
Obesity is a risk factor for stones. Obesity may change the acid levels in the urine, leading to stone formation.
Medical conditions
Some medical conditions have an increased risk of kidney stones. Abnormal growth of one or more of the parathyroid glands, which control calcium metabolism, can cause high calcium levels in the blood and urine. This can lead to kidney stones. Another condition called distal renal tubular acidosis, in which there is acid build-up in the body, can raise the risk of calcium phosphate kidney stones.
Some rare, inherited disorders can also make certain types of stones more likely. Examples include cystinuria, which is too much of the amino acid cystine in the urine, and primary hyperoxaluria, in which the liver makes too much oxalate.
Medication
Some medications, and calcium and vitamin C supplements, may increase your risk of forming stones. Be sure to tell your health care provider all the medications and supplements you take, as these could affect your risk of stone formation. Do not stop taking any of these unless your health care provider tells you to do so.
Family History
The chance of having kidney stones is much higher if you have a family history of stones, such as a parent or sibling.
Diagnosis
“Silent” kidney stones, those that cause no symptoms, are often found when an X-ray is taken during a health exam. Other people have their stones diagnosed when sudden pain occurs while the stone is passing, and medical attention is needed.
When a person has blood in the urine (hematuria) or sudden abdominal or side pain, tests like an ultrasound or a CT scan may diagnose a stone. These imaging tests tell the health care provider how big the stone is and where it is located.
A CT scan is often used in the ER when a stone is suspected. It is used because it can make a quick and exact diagnosis.
Treatment
Treatment depends on the type of stone, how bad it is and the length of time you have had symptoms. There are different treatments to choose from. It is important to talk to your health care provider about what is best for you.
Wait for the stone to pass by itself
Often you can simply wait for the stone to pass. Smaller stones are more likely than larger stones to pass on their own.
Waiting up to four to six weeks for the stone to pass is safe as long as the pain is bearable, there are no signs of infection, the kidney is not completely blocked and the stone is small enough that it is likely to pass. While waiting for the stone to pass, you should drink normal amounts of water. You may need pain medication when there is discomfort.
Medication
Certain medications have been shown to improve the chance that a stone will pass. The most common medication prescribed for this reason is tamsulosin. Tamsulosin (Flomax) relaxes the ureter, making it easier for the stone to pass. You may also need pain and anti-nausea medicine as you wait to pass the stone.
Surgery
- Surgery may be needed to remove a stone from the ureter or kidney if:
- The stone fails to pass.
- The pain is too great to wait for the stone to pass.
- The stone is affecting kidney function. Small stones in the kidney may be left alone if they are not causing pain or infection. Some people choose to have their small stones removed. They do this because they are afraid the stone will unexpectedly start to pass and cause pain.
Kidney stones should be removed by surgery if they cause repeated infections in the urine or because they are blocking the flow of urine from the kidney. Today, surgery usually involves small or no incisions (cuts), minor pain and minimal time off work.
Surgeries to remove stones in the kidneys or ureters are:
Shock wave lithotripsy (SWL)
Shock Wave Lithography (SWL) is used to treat stones in the kidney and ureter. Shock waves are focused on the stone using X-rays or ultrasound to pinpoint the stone. Repeated firing of shock waves on the stone usually causes the stone to break into small pieces. These smaller pieces of stones pass out in the urine over a few weeks.
Because of possible discomfort caused by the shock waves and the need to control breathing during the procedure, some form of anesthesia is often needed. SWL does not work well on hard stones, such as cystine, some types of calcium oxalate and calcium phosphate stones, or very large stones.
With SWL, you may go home the same day as the procedure. You may be able to resume normal activities in two to three days. You may also be given a strainer to collect the stone pieces as they pass. These pieces will be sent to the laboratory to be tested.
Although SWL is widely used and considered very safe, it can still cause side effects. You may have blood in your urine for a few days after treatment. Most stone pieces pass painlessly. Larger pieces may get stuck in the ureter, causing pain and needing other removal procedures.
Ureteroscopy (URS)
Ureteroscopy (URS) is used to treat stones in the kidney and ureter. URS involves passing a very small telescope, called an ureteroscope, into the bladder, up the ureter and into the kidney. Rigid telescopes are used for stones in the lower part of the ureter near the bladder. Flexible telescopes are used to treat stones in the upper ureter and kidney.
The ureteroscope lets the urologist see the stone without making an incision (cuts). General anesthesia keeps you comfortable during the URS procedure. Once the urologist sees the stone with the ureteroscope, a small, basket-like device grabs smaller stones and removes them. If a stone is too large to remove in one piece, it can be broken into smaller pieces with a laser or other stone-breaking tools.
Once the stone has been removed whole or in pieces, the health care provider may place a temporary stent in the ureter. A stent is a tiny, rigid plastic tube that helps hold the ureter open so that urine can drain from the kidney into the bladder. Unlike a catheter or PCNL drain tube, this tube is completely within the body and does not require an external bag to collect urine.
You may go home the same day as the URS and can begin normal activities in two to three days. If your urologist places a stent, he or she will remove it four to 10 days later. Sometimes a string is left on the end of the stent so you can remove it on your own. It is very important that the stent is removed when your health care provider tells you. Leaving the stent in for long periods can cause an infection and loss of kidney function.
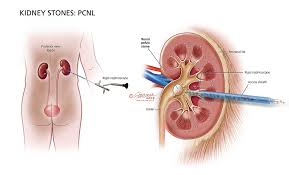
Percutaneous nephrolithotomy (PCNL)
Percutaneous Lithotripsy (PCNL) is the best treatment for large stones in the kidney. General anesthesia is needed to do a PCNL. PCNL involves making a half-inch incision (cut) in the back or side, just large enough to allow a rigid telescope (nephroscope) to be passed into the hollow center part of the kidney where the stone is located.
An instrument passed through the nephroscope breaks up the stone and suctions out the pieces. The ability to suction pieces makes PCNL the best treatment choice for large stones.
After the PCNL, a tube is usually left in the kidney to drain urine into a bag outside of the body. This will allow for drainage of urine and stop any bleeding. The tube is left in overnight or for a few days. You may have to stay in the hospital overnight after this operation.
Your urologist may choose to do X-rays while you are still in the hospital to see if any stone pieces remain. If there are any, your urologist may want to look back into the kidney with a telescope again to remove them. You can begin normal activities after about one-to-two weeks.
Other surgery
Other kidney surgery is rarely used to remove stones. Open, laparoscopic or robotic surgery may be used only if all other less invasive procedures fail.
Why You Get Stones
Part of preventing stones is finding out why you get them. Your health care provider will perform tests to find out what is causing this. After finding out why you get stones, your health care provider will give you tips to help stop them from coming back.
Some of the tests he or she may do are listed below.
Medical and Dietary History
Your health care provider will ask questions about your personal and family medical history. He or she may ask if:
- Have you had more than one stone before?
- Has anyone in your family had stones?
- Do you have a medical condition that may increase your chance of having stones, like frequent diarrhea, gout or diabetes?
Knowing your eating habits is also helpful. You may be eating foods that are known to raise the risk of stones. You may also be eating too few foods that protect against stones or not drinking enough fluids.
Understanding your medical, family and dietary history helps your health care provider find out how likely you are to form more stones.
Blood and Urine Tests
After taking a complete history and doing a physical exam, your health care provider may take blood and urine samples for testing. Blood tests can help find if a medical problem is causing your stones. Your urine can be tested to see if you have a urinary tract infection or crystals that are typical of different stone types. If you are at high risk for getting stones in the future, a 24-hour urine collection can be done. This test will reveal the levels of different stone-forming substances in your urine. The results of this test can help your health care provider recommend make specific diet and medications to prevent future stones.
Imaging Tests
When a health care provider sees you for the first time and you have had stones before, he or she may want to see recent X-rays or order a new X-ray. They will do this to see if there are any stones in your urinary tract. Imaging tests may be repeated over time to check for stone growth. You may also need this test if you are having pain, hematuria (blood in your urine) or recurrent infections.
Stone Analysis
If you pass a stone or a stone is removed by surgery, your health care provider will want to test it. Testing the stone will determine what type of stone it is. This information helps your health care provider decide the best way to prevent future stones.
Prevention of Future Stones
Once your health care provider finds out why you are forming stones, he or she will give you tips on how to prevent them. This may include changing your diet and taking certain medications. There is no “one-size-fits-all” diet for preventing kidney stones. Everyone is different. Your diet may not be causing your stones to form. But there are dietary changes that you can make to stop stones from continuing to form.
Diet Changes
Drink enough fluids each day.
If you are not producing enough urine, your health care provider will recommend you drink at least 3 liters of liquid each day. This equals about 3 quarts (about ten 10-ounce glasses). This is a great way to lower your risk of forming new stones. Remember to drink more to replace fluids lost when you sweat from exercise or in hot weather. All fluids count toward your fluid intake. But it’s best to drink mostly no-calorie or low-calorie drinks. This may mean limiting sugar-sweetened or alcoholic drinks.
Knowing how much you drink during the day can help you understand how much you need to drink to produce 2.5 liters of urine. Use a household measuring cup to measure how much liquid you drink for a day or two. Drink from bottles or cans with the fluid ounces listed on the label. Keep a log, and add up the ounces at the end of the day or 24-hour period. Use this total to be sure you are reaching your daily target urine amount of at least 85 ounces (2.5 liters) of urine daily.
Health care providers recommend people who form cystine stones drink more liquid than other stone formers. Usually 4 liters of liquid is advised to reduce cystine levels in your urine.
Reduce the amount of salt in your diet.
This tip is for people with high sodium intake and high urine calcium or cystine. Sodium can cause both urine calcium and cystine to be too high. Your health care provider may advise you to avoid foods that have a lot of salt. The Centers for Disease Control (CDC) and other health groups advise not eating more than 2,300 mg of salt per day. The following foods are high in salt and should be eaten in moderation:
- Cheese (all types)
- Most frozen foods and meats, including salty cured meats, deli meats (cold cuts), hot dogs, bratwurst and sausages
- Canned soups and vegetables
- Breads, bagels, rolls and baked goods
- Salty snacks, like chips and pretzels
- Bottled salad dressings and certain breakfast cereals
- Pickles and olives
- Casseroles, other “mixed” foods, pizza and lasagna
- Canned and bottled sauces
- Certain condiments, table salt and some spice blends
Eat the recommended amount of calcium.
If you take calcium supplements, make sure you aren’t getting too much calcium. On the other hand make sure you aren’t getting too little calcium either. Talk with your health care provider or dietitian about whether you need supplements. Good sources of calcium to choose from often are those low in salt. Eating calcium-rich foods or beverages with meals every day is a good habit. There are many non-dairy sources of calcium, such as calcium-fortified non-dairy milks. There are good choices, especially if you avoid dairy.
You can usually get enough calcium from your diet without supplements if you eat three-to-four servings of calcium-rich food. Many foods and beverages have calcium in them. Some foods and beverages that might be easy to include on a daily basis with meals are:
Eat plenty of fruits and vegetables.
Eating at least five servings of fruits and vegetables daily is recommended for all people who form kidney stones. Eating fruits and vegetables give you potassium, fiber, magnesium, antioxidants, phytate and citrate, all of which may help keep stones from forming.
A serving means one piece of fruit or one potato or one cup of raw vegetables. For cooked vegetables, a serving is ½ cup. If you are worried you may not be eating the right amount of fruits and vegetables, talk to your health care provider about what will be best for you.
Eat foods with low oxalate levels.
This recommendation is for patients with high urine oxalate. Eating calcium-rich foods (see table above) with meals can often control the oxalate level in your urine. Urinary oxalate is controlled because eating calcium lowers the oxalate level in your body. But if doing that does not control your urine oxalate, you may be asked to eat less of certain high-oxalate foods. Nearly all plant foods have oxalate, but a few foods contain a lot of it. These include spinach, rhubarb and almonds. It is usually not necessary to completely stop eating foods that contain oxalate. This needs to be determined individually and depends on why your oxalate levels are high in the first place.
Eat less meat.
If you make cystine or calcium oxalate stones and your urine uric acid is high, your health care provider may tell you to eat less animal protein.
If your health care provider thinks your diet is increasing your risk for stones, he or she will tell you to eat less meat, fish, seafood, poultry, pork, lamb, mutton and game meat than you eat now. This might mean eating these foods once or twice rather than two or three times a day, fewer times during the week, or eating smaller portions when you do eat them. The amount to limit depends on how much you eat now and how much your diet is affecting your uric acid levels.
Medications
Changing your diet and increasing fluids may not be enough to prevent stones from forming. Your health care provider may give you medications to take to help with this. The type of stone and the urine abnormalities you have will help your health care provider decide if you need medicine and which medicine is best. Common medications include:
Thiazide diuretics
are for patients who have calcium stones and high levels of calcium in their urine. Thiazides lower urine calcium by helping the kidney take calcium out of the urine and put it back in the blood stream. When taking thiazides, you need to limit how much salt you take in, as these medications work best when urine sodium is low.
Potassium citrate
is for patients with calcium stones and low urinary citrate, and for those with uric acid and cystine stones. Potassium citrate makes the urine less acidic or more alkaline (basic). This helps prevent cystine and uric acid stones. It also raises the citrate level in the urine, helping to prevent calcium stones.
Allopurinol
is frequently prescribed for gout, which is caused by high uric acid in the blood. Allopurinol not only lowers the level of uric acid in the blood but also in the urine, so it may also be prescribed to help prevent calcium and uric acid stones.
Acetohydroxamic acid (AHA)
is for patients who produce struvite or infection stones. These stones form because of repeated urinary tract infections (UTI). AHA makes the urine unfavorable for struvite stones to form. The best way to prevent stuvite stones is to prevent repeated UTIs caused by specific types of bacteria and to completely remove the stones with surgery.
Cystine-binding thiol drugs
are used only for patients who form cystine stones. These medications (d-penicillamine or tiopronin) bind to cystine in the urine and form a compound that is less likely than cystine to crystallize in the urine. This drug is used when other measures fail, such as raising fluid intake, reducing salt intake or using potassium citrate.
Vitamin supplements
should be used carefully as some can increase your risk of forming kidney stones. Your health care provider and a dietitian may be good sources of information about over-the-counter nutritional supplements.
Frequently Asked Questions
What is a staghorn stone?
Like the horns of a stag (deer), these stones get their name from the shape they take as they grow to fill the inside of the kidney. Staghorn stones often form because of repeated urinary tract infections (UTIs) with certain kinds of bacteria. Even though they can grow to a large size, you may have no idea you have them because they cause little or no pain. A staghorn stone can lead to poor kidney function, even without blocking the passage of urine. Most often, staghorn shaped stones are the struvite/infection type of stone.
Will my children get kidney stones because I have them?
Kidney stones are more common in people who have a family member with kidney stones. Some conditions that cause stones may be inherited. But sometimes kidney stones form in relatives because of similar diet and lifestyle.
Can kidney stones damage my kidneys?
Yes, but rarely. Kidney stones can cause damage if they cause repeated or serious infection or cause kidney blockage for a long time. Some stones, if left untreated, can cause the kidney to stop working.
Why is it important that I follow up with my health care provider about my kidney stones?
During treatment, your health care provider may ask you to do another 24-hour urine collection and have your blood work checked to see if your urine test results have improved. Your health care provider will also check to see if you are having any side effects from your medications.
If you form stones often, you will need monitoring with X-rays and urine studies to be sure no new stones are forming. Your health care provider will monitor you to make sure your medications and diet changes are working.
How do I manage my kidney stone along with my other health problems, such as diabetes and/or a heart disorder?
Diet changes recommended for heart conditions also often help prevent stones. A healthy diet with lots of fresh fruits and vegetables and less animal protein and salt can help avoid stones and other conditions. You can learn more from your health care provider or dietician. Keeping a normal weight can also help avoid diabetes and stones.
My stone has not passed. Do I need surgery?
If a stone in the ureter does not pass in a reasonable time or is causing pain or infection, you will need surgery to remove it.
What happens if I keep developing stones?
You may get another stone even if you’ve had surgery, changed your diet or are taking medications. However, with the right dietary and medical treatment, you can be less likely to get stones over and over again.
 The Care Up
The Care Up




